Abstract
Cardiac surgery has a risk for extensive blood loss which poses a particular challenge in individuals refusing blood transfusions. Additionally, preoperative anemia with a hemoglobin (Hb) below 13 g/dL in men and 12 g/dL in women is associated with increased short and long-term complications and mortality and increases the need for blood transfusion support. The current guidelines for perioperative anemia management recommend optimizing hemoglobin levels prior to surgery and utilizing blood conservation techniques during the procedure. At present red blood cell (RBC) transfusions during cardiac surgery are usually recommended when Hb levels are below 7-8 g/dL a restrictive transfusion strategy to reduce complications. However, the use of any RBC transfusions is associated with worse outcomes in cardiac surgery compared with those who do not receive transfusions.
We have found that JW seek out quality health care and accept the vast majority of medical treatments once they are educated. The Transfusion Free Medicine Coordinator's role in the Anemia Clinic is to endorse clinical strategies for managing hemorrhage and anemia without blood transfusion. They educate and counsel the patients so they can decide as to what blood fractions and cell salvage techniques they will accept. We have found that some Health Care Providers are unaware that ESAs also contain albumin so JW patients may be given this product without that knowledge. The vast majority of patients will accept the use of ESAs but find the cost prohibitive.
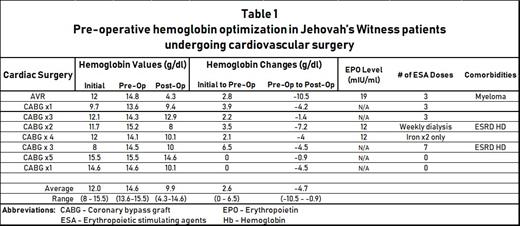
Jehovah's Witness patients have provided a natural case study for examining how well adjuvant therapies can improve preoperative anemia without transfusions and continue with good outcomes. Hb optimization is achieved through the use of intravenous iron and, if needed, erythropoiesis stimulating agents (ESAs). In Table 1 we highlight our single center data in which all cardiovascular surgeries were performed by a surgeon experienced in blood-conservation strategies. Our thirty-day re-admission rates for all patients was zero percent, compared to state-specific data, which estimates about an 11.7% rate of re-admission. The data illustrate the need to have a target Hb 13 or above to allow for the decline that may occur during the hospital stay. Of note no thromboembolic events have occurred with the use of an ESA in this group.
Although ESAs are approved to optimize Hb in orthopedic surgery, they are not covered for cardiac surgery which has presented a significant challenge to patients who can not safely proceed to surgery until a target Hb between 13 to 15 g/dL is achieved.
These data highlight the utility and safety associated with the use of ESAs for patients who do not accept blood products at an experienced Center for Transfusion-Free Medicine, such as ours. At this time, since insurance companies do not cover the cost of ESAs for patients needing life-saving cardiovascular operations, cost is a prohibitive barrier for patients. Unfortunately, it is not uncommon for patients to have to borrow money from others or set up payment plans. We hope that analyses like ours will help drive changes in reimbursement policies, particularly for patients who based on religious convictions, cannot receive blood products, and thus for whom pre-operative hemoglobin optimization is of utmost importance.
No relevant conflicts of interest to declare.
Erythropoiesis-stimulating agent (ESA) are indicated for the treatment of anemia due to Chronic Kidney Disease in patients on dialysis and not on dialysis, Zidovudine in patients with HIV-infection, anemia due to myelosuppressive chemotherapy and reduction of allogeneic RBC transfusions in patients undergoing elective, noncardiac, nonvascular surgery